
Sleep and Sleep Problems
Overview
Sleep is vital to concussion recovery. It is your brain’s primary mechanism for healing and can be a predictor of how long concussion symptoms will persist.
Almost 60% of concussion patients experience chronic sleep difficulties, making sleep disturbances three times more common in concussion patients than in the general population. This is because concussions alter crucial processes that enable the brain to sleep and wake up. Concussion patients often experience a frustrating cycle of sleep problems that slow their healing progress, which in turn contributes to further sleep problems.
Despite the difficulty of the post-concussion sleep experience, recent breakthroughs in sleep research indicate that, through following correct guidelines and receiving appropriate treatment, resolving sleep disturbances after concussion is possible.
Timeline of Sleep After Concussion
1-3 days post-concussion
Sleep is critical in the first few days after a concussion for the repair of white matter, a network of nerve fibers in the brain that is crucial to overall cognitive health.
In the first one to three days after injury, allow a concussion patient to sleep, even during the day. It is not necessary to wake a concussion patient up every few hours if they are sleeping.
That being said, patients should not completely “cocoon,” even in the first 24-48 hours. It is outdated advice to lie down in the dark during the day for extended periods, and this can impede recovery. Activities of daily living, such as light walking, preparing a meal, and calm socializing, are recommended in the days following a concussion.
For more guidelines on the first days after a concussion, see our Guidelines for Recovery page.
3 days- 4 weeks post-concussion
After the initial period of 1-3 days, sleeping during the day is not recommended. Patients should begin to increase their physical and cognitive exercise as tolerated, particularly in the first two hours after waking up. They should also ensure that they are practicing good sleep hygiene and Self Care for Sleep.
Sleep disturbances can begin to appear in the weeks after a concussion because during this period, the injured brain is attempting to re-establish its regular sleep-wake cycle. Mental health symptoms of concussion that affect sleep also tend to present during this time. See our section on the causes of sleep disturbances after concussion for more information.
*If a sleep disturbance appears during the first 10 days after a concussion, consider seeking treatment. The quality of sleep during the first 10 days after a concussion is associated with increased risk of persisting symptoms.
For information on sleep disturbance treatment, see our Treatment Options and Finding A Provider pages.
No later than 4 weeks post-concussion
If a patient is still experiencing persisting symptoms, including sleep disturbances, 4 weeks after their concussion, it is recommended that they seek a comprehensive assessment of their symptoms. Ideally, this involves evaluation by a team of medical professionals with different backgrounds.
For information on comprehensive treatment, see our Overview of Treatments and Self-Care page.
Seeking treatment for sleep disturbances earlier than 4 weeks after a concussion may reduce the risk of persisting symptoms.
For information on sleep disturbance treatment, see our Treatment Options and Finding A Provider pages.
The Role of Sleep
Sleep is a fundamental physiological process that plays a crucial role in overall health, cognitive function, and emotional well-being. Most adults need 7 to 9 hours of sleep per night to maintain peak performance. Deprivation of this nightly sleep could negatively impact executive functions such as concentration, decision-making, and problem-solving. Regarding concussion recovery, the relationship between sleep and the healing process is particularly noteworthy. Concussions disrupt the brain’s normal functioning, leading to a cascade of biochemical and metabolic changes. Adequate sleep becomes essential for the brain to repair itself and for the body to support this intricate healing process.
During sleep, the brain undergoes essential processes that contribute to physical and cognitive recovery. For individuals recovering from a concussion, quality sleep is especially vital as it allows the brain to focus on repairing damaged neural connections. Sleep disturbances can exacerbate concussion symptoms and reduce recovery potential.
Sleep difficulties can influence the number of days to concussion symptom recovery. A study evaluating the sleep duration and quality of 17 college-aged students experiencing concussions found that longer wake time throughout the night and less sleep efficiency were associated with longer recovery time. In addition, “poorer post-concussion sleep quality was correlated with longer recovery.”
Other studies support and expand upon these findings. One retrospective chart review at a concussion clinic examined sleep disturbance and concussion duration in adolescent patients over seven years. Of the 417 patients included, one-third reported disturbance in sleep, which was associated with “a 3- to 4-fold increase in recovery time.” Furthermore, sleep disturbance occurred significantly more following non-sport-related concussions compared to sport-related concussions.
Due to the implications that sleep difficulties have for concussion recovery time, clinicians treating concussion patients should check for sleep disorders. They may recommend melatonin, which has been shown to help alleviate sleep disturbance in those recovering from a concussion but should only be used for a short time. To learn more about ways to promote sleep, visit our self-care page on sleep.
Causes of Sleep Disturbances After Concussion
Physical symptoms
Prolonged physical symptoms of concussion, such as headaches, neck pain, light sensitivity, and noise sensitivity, can lead concussion patients to experience more physical distress than they experienced before their injury. Physical distress triggers the release of signals, such as norepinephrine, that prompt wakefulness in the brain. Physical pain has been significantly associated with sleep problems.
Mental health symptoms
Concussions have a profound impact on a patient’s mental health. Concussion patients often experience new or exacerbated mental health symptoms, such as anxiety, depression, mood swings, or Post Traumatic Stress Disorder after their injury. These changes can impact sleep significantly.
In particular, patients experiencing a combination of concussion and PTSD have been found to suffer significant sleep disturbances. White matter alterations in patients with concussion and PTSD are associated with these difficulties. Good white matter integrity is critical to the brain’s ability to perform tasks such as signal and memory processing, executive functions, and REM sleep.
Circadian rhythm alteration
The circadian rhythm is the body’s “internal clock,” a repeating 24-hour cycle that guides the activity of various systems, including temperature regulation, appetite, and sleep. This cycle is often altered after a concussion because concussions are frequently followed by less exercise and more daytime rest. The time it takes for a body to re-orient its circadian rhythm varies from person to person, and sleep-wake cycles in concussion patients may take a while to regulate.
Chemical factors
The brain experiences sleep and wakefulness as a result of a complex orchestration of neurotransmitters, chemical messengers that carry signals between neurons. An injury can disrupt this intricate communication system; damaged neurons are less able to receive and release signals.
As a result, certain chemicals that compel the brain to start or stop sleep, such as serotonin, histamine, and norepinephrine, may not be released in their usual patterns after a brain injury.
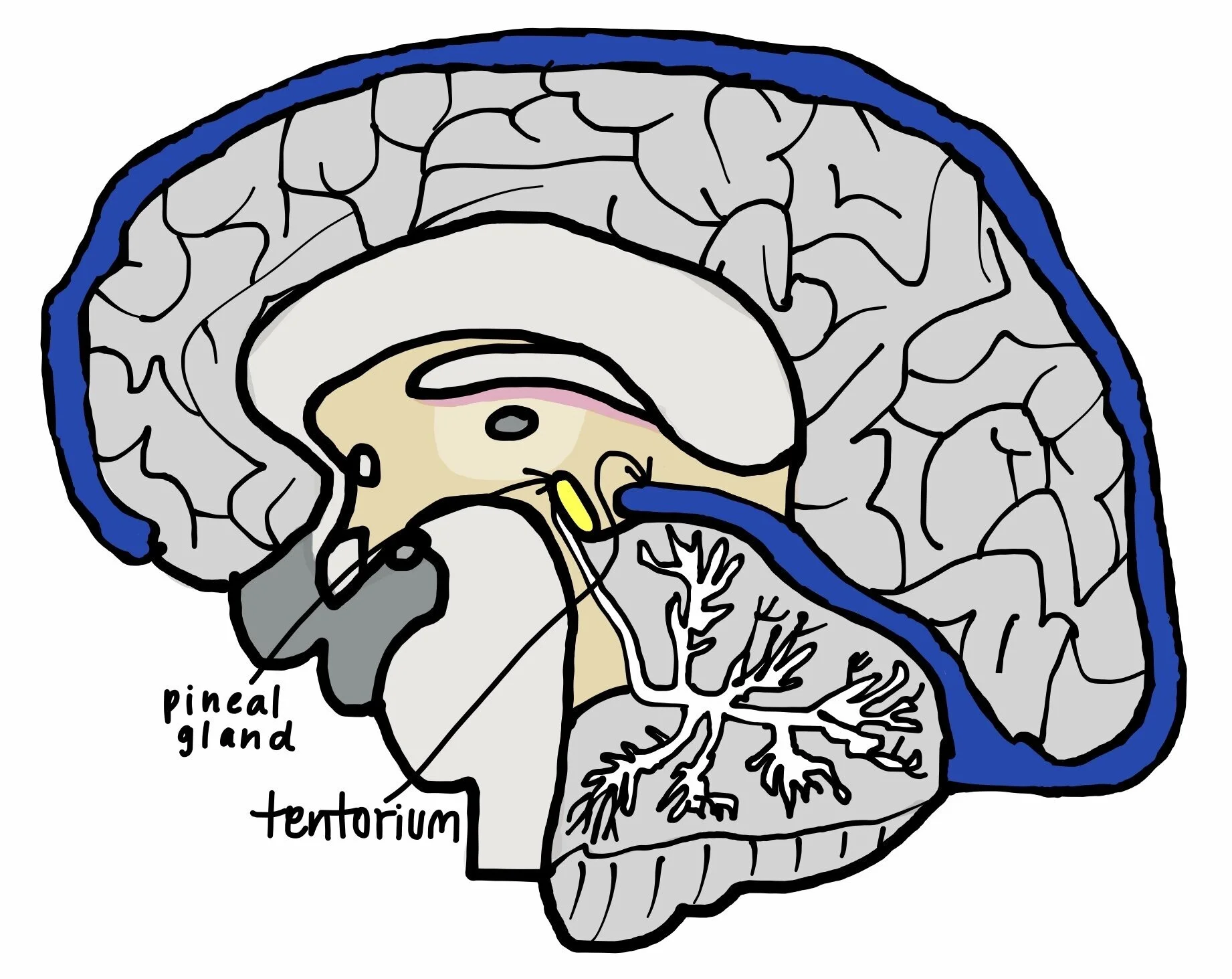
Structural factors
Concussion patients may suffer sleep disturbances as a result of structural changes that occur with injury. Concussion patients have been found to experience an increased proximity between their tentorium, a brain region covering the top of the cerebellum, and their pineal gland, a small region in the center of the brain that secretes melatonin. This increased proximity has the potential to disrupt the flow of melatonin, a hormone that is critical to initiating sleep.
Concussion patients with sleep disorders tend to have longer tentoriums than concussion patients without. Image drawn by Bethany Lazo, summer 2021 Concussion Alliance intern.
Concussion-Related Sleep Disorders
Concussions can trigger or worsen the following sleep disorders.
Sleep Apnea
Sleep apnea is a sleep disorder characterized by interruptions in breathing or very shallow breathing during sleep. These pauses in breathing, lasting 10–120 seconds and occurring 20–30 times or more per sleeping hour, lead to decreased oxygen levels in the blood. Sleep apnea symptoms include excessive daytime sleepiness, mouth breathing, and snoring.
Sleep apnea manifests in two primary forms: obstructive sleep apnea (OSA) and central sleep apnea. OSA results from a physical blockage of the airway, typically caused by relaxed throat muscles and tissues, while central sleep apnea stems from a failure of the brain to signal the muscles to breathe. OSA occurs much more frequently than central sleep apnea in concussion patients. One study found that those with a history of concussion had an 18.6% higher prevalence of sleep apnea than the general adult population.
In a study examining the sleep of veterans with a history of TBI/concussion, sleep apnea was one of the two most common sleep disorders reported. 92.9% of veterans with sleep apnea had OSA. In another study, OSA had an increased incidence in post-concussion syndrome (PCS) patients; 78% of participants in this study were diagnosed with sleep apnea. These individuals experienced more memory symptoms, non-restorative sleep, and headaches after waking up than PCS patients without sleep apnea.
Given that sleep apnea could worsen concussion recovery and lead to cognitive dysfunction, a concussion patient who thinks they might have sleep apnea should seek appropriate treatment from a medical provider. A CPAP machine could assist OSA patients with breathing at night.
Insomnia
Insomnia is characterized as having trouble falling asleep or staying asleep or having unrefreshing sleep despite having ample opportunity to sleep. These disturbances can be transient, lasting for a few nights, or chronic, persisting for weeks or months. Insomnia can lead to daytime fatigue, impaired concentration, mood disturbances, and a diminished overall quality of life. 40-65% of concussion patients experience symptoms of insomnia. Adolescents are especially prone to insomnia following concussion due to “physiologic changes and increased societal and academic demands.”
Repeated concussions may heighten the risk and severity of Insomnia. Insomnia can also increase the likelihood of future concussions, given that sleep deficiency could precipitate accidents like car crashes. Beyond that, insomnia symptoms tend to extend the duration of a concussion since these individuals require sleep during recovery.
While other sleep disorders do not usually correlate with a specific severity of TBI, Insomnia appears more frequently in concussion patients than in those with moderate or severe TBI. This relationship could be explained by the elevated pressure for those with concussions to return to normal functioning, which may consequently raise stress levels and cause sleep problems. Patients with insomnia may benefit from blue-light therapy and cognitive behavioral therapy.
Hypersomnia
Hypersomnia refers to excessive time spent sleeping or sleepiness during the day. Hypersomnia is common following concussion, particularly in the days right after the impact. It is normal to rest during this time. Some patients, however, continue to experience persistent daytime sleepiness post-injury. Patients with hypersomnia often find it challenging to maintain alertness during waking hours, which can adversely affect their daily functioning, cognitive abilities, and overall quality of life.
Following a concussion, the brain undergoes physiological changes that can impact sleep patterns. Hypersomnia may manifest as a direct result of the brain's attempt to recover from the injury. The trauma incurred during a concussion can disturb the intricate neural networks responsible for regulating sleep. It can damage hypocretin-producing hypothalamic cells, which regulate sleep. Injury to these cells may lower hypocretin levels and make one feel more tired.
PTSD, physical injuries, and depression can worsen hypersomnia symptoms. The FDA has not approved any medications to treat concussion-related hypersomnia specifically, but doctors may prescribe pharmaceuticals off-label to reduce excessive sleepiness. These include modafinil, armodafinil, and amphetamines. That said, the evidence supporting the efficacy and safety of these drugs in concussion patients is mixed. Individuals with concussions can also use morning bright light therapy to reduce fatigue if they prefer nonpharmacologic interventions. Our blog has more information on the benefits of morning blue light exposure.
Circadian Rhythm Sleep-Wake Disorders
Circadian Rhythm Sleep-Wake Disorder (CRSWD) is a common yet often overlooked aspect of the sleep-wake cycle. This disorder is characterized by disruptions in the body's internal biological clock, known as the circadian rhythm, which regulates the sleep-wake cycle and various physiological processes over a 24-hour period.
Following a concussion, individuals may experience disturbances in their circadian rhythm, leading to difficulties falling asleep, staying asleep, or maintaining a regular sleep pattern. A study of people who had experienced concussion and reported chronic insomnia found that 26% of participants had a CRSWD. The most common circadian diagnosis was delayed sleep-wake phase disorder.
Three primary types of CRSWDs warrant attention in the context of concussion recovery:
Delayed Sleep Phase Syndrome (DSPS): This disorder manifests as a delayed onset of sleep, making it challenging for individuals to adhere to a consistent sleep schedule—a crucial component of concussion recovery.
Advanced Sleep Phase Syndrome (ASPS): ASPS leads to an earlier-than-normal onset of sleep and waking up, resulting in daytime sleepiness and fatigue, which can hinder cognitive functioning during recovery.
Irregular Sleep-Wake Rhythm Disorder: Characterized by fragmented sleep patterns, this disorder disrupts the traditional sleep-wake cycle, potentially compromising the quality of rest vital for concussion healing.
Addressing CRSWDs during concussion recovery necessitates a comprehensive approach. Implementing proper sleep hygiene practices, establishing consistent sleep routines, and creating optimal sleep environments are fundamental strategies. Additionally, light therapy, involving exposure to natural light during the day and minimizing artificial light exposure at night, can aid in synchronizing the internal body clock.
Acknowledging and actively managing CRSWDs is crucial for individuals navigating the complex terrain of concussion recovery. By addressing these sleep-wake disorders, individuals can enhance their overall well-being, promote cognitive healing, and foster a smoother journey toward full concussion recovery. It is recommended to see a healthcare provider for sleep dysfunction after 10 days.
Sleep Hygiene Tips
Sleep hygiene is a treatment in clinical sleep medicine that includes a set of behavioral and environmental recommendations to promote healthy sleep and improve cognitive performance. The following tips from the National Institutes of Health could help advance restorative sleep during concussion recovery:
Source: Max Pixel, “Education.” Accessed via https://www.maxpixel.net/photo-4095953 CC0.
Sleeping environment/habits
Keep your sleeping area dark, comfortable, tidy, and quiet. Turn off any sources of light in the bedroom. You may consider playing neutral or natural music or white noise to block out distracting sounds.
Keep a consistent sleep schedule by going to bed and waking up at around the same time every night and morning. It may be especially helpful to wake up at the same time every day, as this can help your whole schedule fall into place.
Getting enough sleep at night can assist the recovery process. Children (6-12 years) need 10-11 hours of sleep per night. Adolescents (13-18 years) require 9-9.5 hours of sleep per night. Adults are advised to get 7-9 hours of sleep per night.
Try not to nap during the day—especially after 3 PM—to avoid struggling to fall asleep at night. If napping is unavoidable, restrict naps to no longer than one hour.
Reserve your bedroom for sleeping. Other entertainment activities, such as playing games, using your phone, or watching movies, should happen in another room. No electronic equipment should be stored in the bedroom. If unable to remove electronics from the sleeping area, shut off your computers, tablets, and cell phones (or put them in sleep mode) to ensure uninterrupted sleep.
Lifestyle
Avoid stimulants such as caffeine and nicotine. The effects of stimulating foods and beverages can take up to eight hours to fully wear off.
Avoid alcoholic beverages for four hours before bed. While alcohol may help you fall asleep, it often prevents you from entering the restorative stages of sleep. Additionally, once the sedating effects of the alcohol wear off, you may wake up.
Avoid eating heavy meals late in the evening. Large meals may cause indigestion, which interferes with sleep, and eating late at night can interfere with your circadian rhythm.
Regular exercise helps promote sleep at night and improve health conditions. However, vigorous exercise within three hours of bedtime is not recommended.
If you have difficulty sleeping, having a warm bath or massage before bed might help. Other recommended activities like reading, listening to soft music, or doing something relaxing can help you put your mind at ease and fall asleep.
Avoid using screens within two hours of sleeping. Additionally, close screens like laptops, phones, tablets should be switched into nightmode when the sun sets, this is more effective at blocking blue light than blue light blocking glasses.
Avoid medications that delay or disrupt sleep. Some prescription heart and blood pressure medications and over-the-counter cold and allergy medications can disrupt sleep patterns.
Ensure proper nutrition. The body needs sufficient vitamin and mineral intake to produce melatonin, which makes you sleepy. Include iron, magnesium, and B vitamins in your diet.
Treatment Options
Beyond practicing good sleep hygiene, there are various treatment options for post-concussion sleep disorders.
Options through a healthcare provider
CBT-I
Cognitive Behavioral Therapy for Insomnia (CBT-I) is a highly effective, accessible, non-pharmacological treatment for concussion patients struggling to fall asleep. Standard CBT-I treatment is six to eight counseling sessions. Depending on the provider, sessions can range from thirty to ninety minutes each.
CBT-I patients have been found to demonstrate significant improvement, both during treatment and in the long term.
See Finding a Provider to find a CBT-I specialist.
Medication
Depending on the disorder and patient, a provider may prescribe medication for sleep difficulties. See Finding a Provider for more information on starting this process.
Disorder specific treatments
In some cases, there are specific treatments for sleep disorders that a provider may recommend. For example, CPAP machines are available for patients with Sleep Apnea. Our Concussion-Related Sleep Disorders section has more information about these specific treatments.
Options that do not require a healthcare provider
CBT-I Apps
App-based Cognitive Behavioral Therapy for Insomnia has also been effective for patients struggling with Insomnia. For more information on CBT-I apps, see our Self-Care page on CBT-I resources
Light Therapies
Blue light therapy
Studies have found that blue light therapy is another non-pharmacological treatment that is associated with significant improvement in insomnia patients after concussion. It has also been associated with improvement in sleep-wake disorders. The therapy involves controlled exposure to blue light in patients’ first two hours of being awake. It is important to note that blue light exposure later in the day is not beneficial to falling asleep
NIR
Near-Infrared Light (NIR) is an emerging treatment involving exposure to controlled near-infrared light before bed. The therapy has been linked to improvement in insomnia patients.
CBD
CBD and CBD+THC have been found to assist with sleep disturbances, primarily with decreasing patients’ time to fall asleep. They also have been found to relieve other symptoms that contribute to sleep disturbances, such as pain and anxiety. However, CBD+THC has been observed to reduce time in REM, a stage of sleep important for memory, restfulness, and healing.
Check your state guidelines and talk to a medical professional before beginning to use CBD or CBD+THC. See our page Cannabis for Concussions for more information.
Electroacupuncture
Research has linked electroacupuncture to increased sleep quality in concussion patients who struggle with insomnia, particularly those who struggle with post-injury depression. Electroacupuncture involves inserting thin needles into the body that carry electrical current. Details of the treatment may vary depending on the provider, but one studied example of post-concussion electroacupuncture involved thirty-minute sessions three days a week for eight weeks.
When to See a Specialist
It is important to see a sleep specialist if a sleep disturbance lasts longer than four weeks after a concussion. Conditions that require professional attention include:
Any concussion-related sleep disorders mentioned above
Narcolepsy: Extreme drowsiness causing one to suddenly fall asleep at inappropriate times.
Restless legs syndrome (RLS): Uncontrollable urge to move the legs because of uncomfortable sensations, often when lying down.
Bruxism: Teeth grinding or jaw clenching.
Periodic limb movement disorder (PLMD): Involuntary jerking or twitching of the arms and legs during sleep.
Sleepwalking: Walking around or performing tasks while asleep and lacking awareness of it.
Delayed sleep phase syndrome: Sleep patterns delayed by at least two hours.
Finding a Provider
A sleep specialist is a doctor who has the ability to diagnose and treat multiple sleep disorders. There are many sleep specialists in locations nationwide available to help. Some work in private practice, while others work in hospitals or sleep centers.
Your first step should be contacting your primary care doctor for a referral to a sleep specialist for an evaluation. After collecting a few names of recommended doctors, you can do a quick Internet search to verify their specialty in a particular sleep issue or simply look for any positive or negative feedback.
If you’d prefer seeing a sleep specialist without the help of your doctor or insurance provider, you can find an accredited sleep center through organizations such as:
Psychology Today Therapist Directory
To get the most personalized results, you should use relevant keywords such as “sleep specialist” and enter the zip code of your current location.
In preparation for your visit, you may consider keeping a sleep diary for a few weeks before arriving at your appointment. That way, the specialist can examine your record of symptoms and quickly diagnose and propose a treatment plan. It is imperative to find a specialist who makes you feel safe and comfortable. They should make note of your symptoms and listen to your concerns. If you have any questions about a certain sleep study or treatment plan, do not hesitate to ask them during your visit.
















In this New York Times article, Christina Caron discusses one of the most effective therapy treatments: Cognitive Behavioral Therapy (CBT). However, it’s not only used in clinical psychology––but also to treat a common experience: insomnia. Most people have experienced insomnia at one point in their life or another. However, for some, insomnia is a constant in their lives; one in 10 adults has chronic insomnia, and it is a common symptom after a concussion.