Athletic Trainers
Overview
Oftentimes people think athletic trainers are just for athletes, but they actually can provide a range of medical and rehabilitative services in a variety of environments, such as schools, rehabilitation centers, physical therapy centers, and even sometimes workplaces. Athletic trainers are multi-skilled healthcare professionals who often collaborate with a team of other medical professionals, such as physicians, to provide healthcare services. ATs administer baseline testing and are often the first to evaluate for potential concussion. Depending on state laws, ATs may not be able to officially diagnose concussions or medically clear patients to return to work, school, or sport. ATs can also implement a rehabilitation program to help the patient's injuries and prevent future re-injury. It should be noted that care is not always consistent. State regulations differ across the United States and Canada, so there can be limits to what an AT can do.
ATs who undergo extensive training programs often have considerable knowledge of concussion and rehabilitation practices; however, every AT is different. Some ATs may have less knowledge pertaining to concussion than others, so it is important to ask questions and do some research beforehand when possible.
Studies have shown that the presence of an AT can often benefit high school and college sports. There are disparities in concussion reporting, diagnosis, and care between schools that can afford ATs and those that cannot.
What are Athletic Trainers?
According to the National Athletic Trainer’s Association (NATA), “Athletic trainers are highly qualified, multi-skilled health care professionals who render service or treatment, under the direction of or in collaboration with a physician, in accordance with their education, training and the state's statutes, rules and regulation.” While they are sometimes part of health care teams (such as sports medicine teams), they are often the first ones to recognize and diagnose concussions, conduct examinations, and implement therapeutic intervention and rehabilitation of injuries such as concussion. ATs also play a crucial role in creating injury prevention plans for their patients.
When you’d work with an AT
Workplace and other settings
ATs provide medical services to all types of patients in various settings, and do not just care for athletes. In some industrial workplaces, employers have found that having an AT employed on-site can result in faster diagnosis and creation of rehabilitation programs that help workers return to work. On-site diagnosis and care can be more efficient, since those workers do not have to travel to an appointment with an outside healthcare provider.
Another place ATs can be found is in sports medicine clinics where a multitude of different patients can be treated. Typically, patients working with ATs at these clinics are referred there by a physician or another AT from a school sport.
High school and college sports
In both high school and college sports, ATs are sometimes part of a sports medicine team that helps provide care for athletes. During rehabilitation, ATs can help patients design injury prevention plans, combining risk reduction with rehabilitation and strengthening to reduce patients’ risk for reinjury in the future.
Programs created by ATs can also shorten rehabilitation time, which can have positive results and less absentee time from work, school, and sport. Shortened rehabilitation time can result in reduced health care costs.
What to expect when working with an AT
Athletic trainers work in a multitude of environments, and are often the first line of defense for injuries. Athletic trainers are best positioned in any area where people are active, whether that be a school environment, a workplace, or the military.
When you see an athletic trainer, they will likely first ask you about your injury and the symptoms you're experiencing. For a concussion, an AT will run diagnostic tests including follow-up baseline testing (to compare against your previous baseline test), balance tests, and vestibular ocular assessments. You can then expect information on what exercises will make up your rehabilitation program.
Athletic trainers also often work closely with other healthcare and sports professionals, including sports medicine doctors, strength and conditioning coaches, physical therapists, and other athletic trainers. However, it depends on the setting as some athletic trainers work without assistance from other specialists. In most states, there's a mandatory referral program for concussions that athletic trainers must follow before return to play. This means in many states a physician or licensed healthcare professional must sign off for the athlete to return to play, although some states allow ATs to diagnose concussions and clear athletes to return to play.
What kind of schooling/training do athletic trainers have?
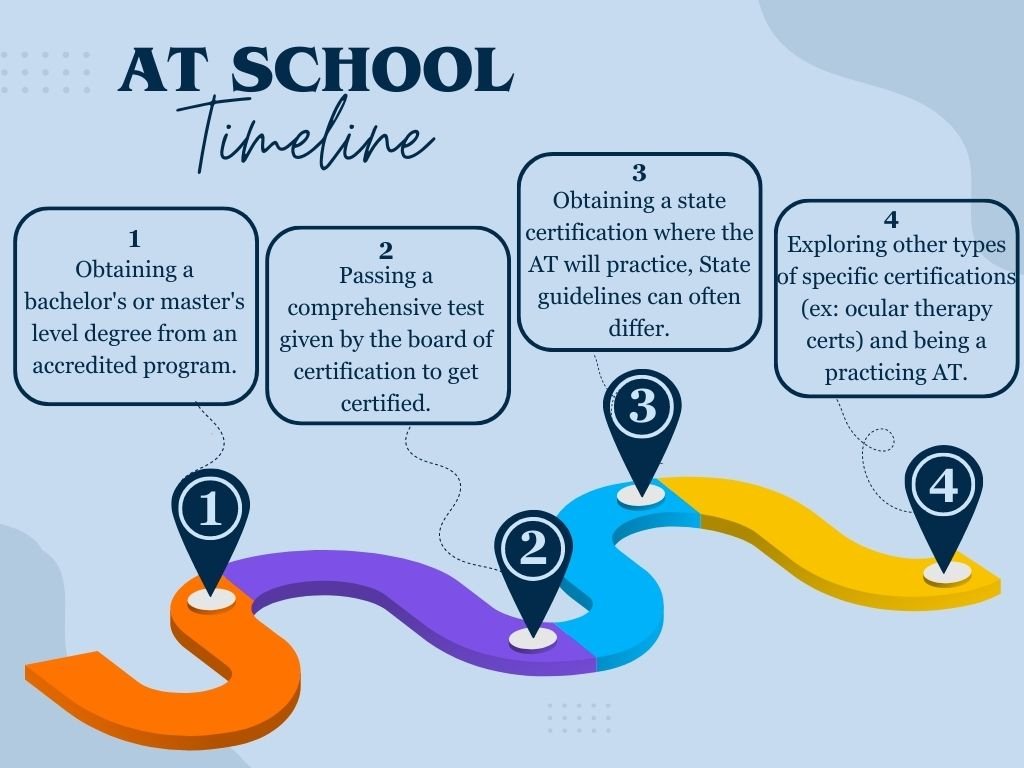
Currently, all ATs must graduate from an accredited program at a master’s degree level; however, those who are older and already practicing may only have a bachelor's degree, as the master’s requirement is a newer development. Once the degree is completed, the AT must pass the Board of Certification test to obtain the Athletic Trainer Certified (ATC) designation. ATs are also responsible for obtaining a certification in the state they choose to work in. It should be noted that not every state has the same guidelines concerning what types of certifications are necessary to be a practicing AT, and what services the AT can provide.
ATs are licensed and regulated in the United States and District of Columbia. Forty-nine states (all US states excluding California), as well as the District of Columbia require ATs to hold the Board of Certification credential of “Athletic Trainer Certified” (ATC) . Learn more about the certification of athletic trainers here.
What kind of education do athletic trainers have with concussions?
It is crucial that all concussion patients do their best to educate themselves before working with an AT or medical provider, so they can advocate for themselves. Having a basic understanding of the concussion/ rehabilitation practices can help better the care you receive.
With concussion, today’s masters programs have done a great job with concussion-focused knowledge and practices, as ATs can take many different types of classes relating to concussion care.
However, it should be noted that this has not always been the case. ATs from older generations may not be up to date with current concussion guidelines, and also are not required to get newer certifications that incorporate current best practices.
A recent study showed that “sports officials’ and athletic trainers’ concussion knowledge, attitudes, and behavioral intentions improved immediately following completion of the CDC HEADS UP online training.” The HEADS UP online concussion training course was created by the Center for Disease Control and Prevention with the purpose of spreading education surrounding concussion. The “CDC HEADS UP online training course for youth sports coaches includes learning objectives aimed at improving: (1) understanding of concussion and its potential consequences; (2) recognition of concussion signs and symptoms and how to respond; (3) coaches’ ability to implement return to activity (sports and school) steps after a concussion; and (4) focus on concussion prevention and preparedness.”
How knowledgeable are athletic trainers about referrals to additional care?
All states, except Wyoming, have laws that govern return-to-play protocol for athletes. These laws address whether medical clearance is required before returning to play and what kind of healthcare professional can give that clearance. Oftentimes that involves a mandatory referral to a physician before return-to-play, according to Colorado Association of Athletic Trainers President Jeb Davis. In states where athletic trainers cannot sign off on return-to-play, they work in concert with the professions that can–often a physician. Learning about return-to-play pathways is a mandatory part of becoming an athletic trainer. Athletic trainers are often involved in decision-making around referrals to other providers, including providing insights based on regular monitoring and assessments of the patient. The next steps may include referrals to a physical therapist, an occupational therapist, or a physician
What concerns are there with AT knowledge in concussion?
Athletic trainers, especially those stationed in athletics environments, often see numerous concussions, so they tend to have extensive experience with concussions. Although many athletic trainers have an up-to-date and thorough knowledge of the care and treatment of concussions, not all do. A recent study showed that the longer an athletic trainer worked, the less strictly they followed proper guidelines. Additionally, another study showed that while current best practices recommend a “3-domain concussion-assessment–battery approach” that includes at minimum a symptom checklist, balance assessment, and neurocognitive examination, nearly half of athletic trainers were assessing less than three domains when making return to participation assessments. Even many medical professionals may not have complete knowledge of concussion management as medical students get a limited amount of concussion education during their schooling. This gap in knowledge for athletic trainers and other medical professionals can lead to incomplete concussion protocols for athletes.
Athletic trainers in team environments can be under considerable pressure from coaches. A survey of athletic trainers in NCAA programs found that more than a third reported that coaches had an influence on the hiring and firing of ATs, and 58% of respondents stated that they had been “pressured… to make a decision that was not in the best interest of a student athlete’s health.” This means student athletes may return to play before their body and brain are fully healed, putting them at risk for prolonged recovery and further injury.
Explore the relationship between the presence or lack of athletic trainers and disparities in concussion care, particularly racial and gender disparities.
Athletic trainers are critical to proper concussion care in many school and team environments. A clear relationship exists between the lack of athletic trainers available to a team and gaps in concussion diagnosis and proper treatment. A study that looked at Oregon schools with and without athletic trainers found that schools with athletic trainers screened more students and were more able to identify concussions and reduce injury rates. Additionally, a recent survey found that high school athletes with access to athletic trainers had more concussion knowledge.
The burden falls hardest on small and small-budget schools that cannot afford to hire athletic trainers. Researchers recently conducted a study on the difference in concussion care between Title I schools and non-Title I schools. Title I schools have a high student poverty rate, lower funding, and are less likely to have a full-time athletic trainer. The study authors included the term bell-ringer in their survey to “determine athletes’ perception of the seriousness in terminology and to assess when a possible concussion may have occurred.” The study showed that “a larger proportion of Black athletes who experienced bell-ringers and concussions did not report them to an authoritative figure compared with White athletes.” Considering other studies’ findings that ATs improve concussion knowledge and reporting, the lack of ATs in Title I schools could contribute to the disparity in concussion reporting observed in this study.
Female-dominant activities such as cheerleading, competetive dance, and other performance athletics are not always classified as officially-recognized sports. ATs are less likely to be present at practice or other competitions meaning injuries including concussions are “underreported to the ATs… and it is not mandated that the athlete obtains return-to-play clearance.”