Autonomic Nervous System (ANS) Dysfunction
M Nadir Haider, MD, from University at Buffalo's Concussion Management Clinic, has reviewed this page for content accuracy. haider@buffalo.edu
Contents
What is the Autonomic Nervous System (ANS)?
Potential diagnostic tools for ANS dysfunction
What treatment/therapy options do I have?
What happens to the brain at the cellular/molecular level when ANS dysfunction is present?
One of the many potential factors contributing to persistent post-concussion symptoms is autonomic nervous system (ANS) dysfunction. Unfortunately, most people who experience ANS dysfunction do not recognize its symptoms, such as anxiety/depression, irregular heart rate, exercise intolerance, and sweating abnormalities.
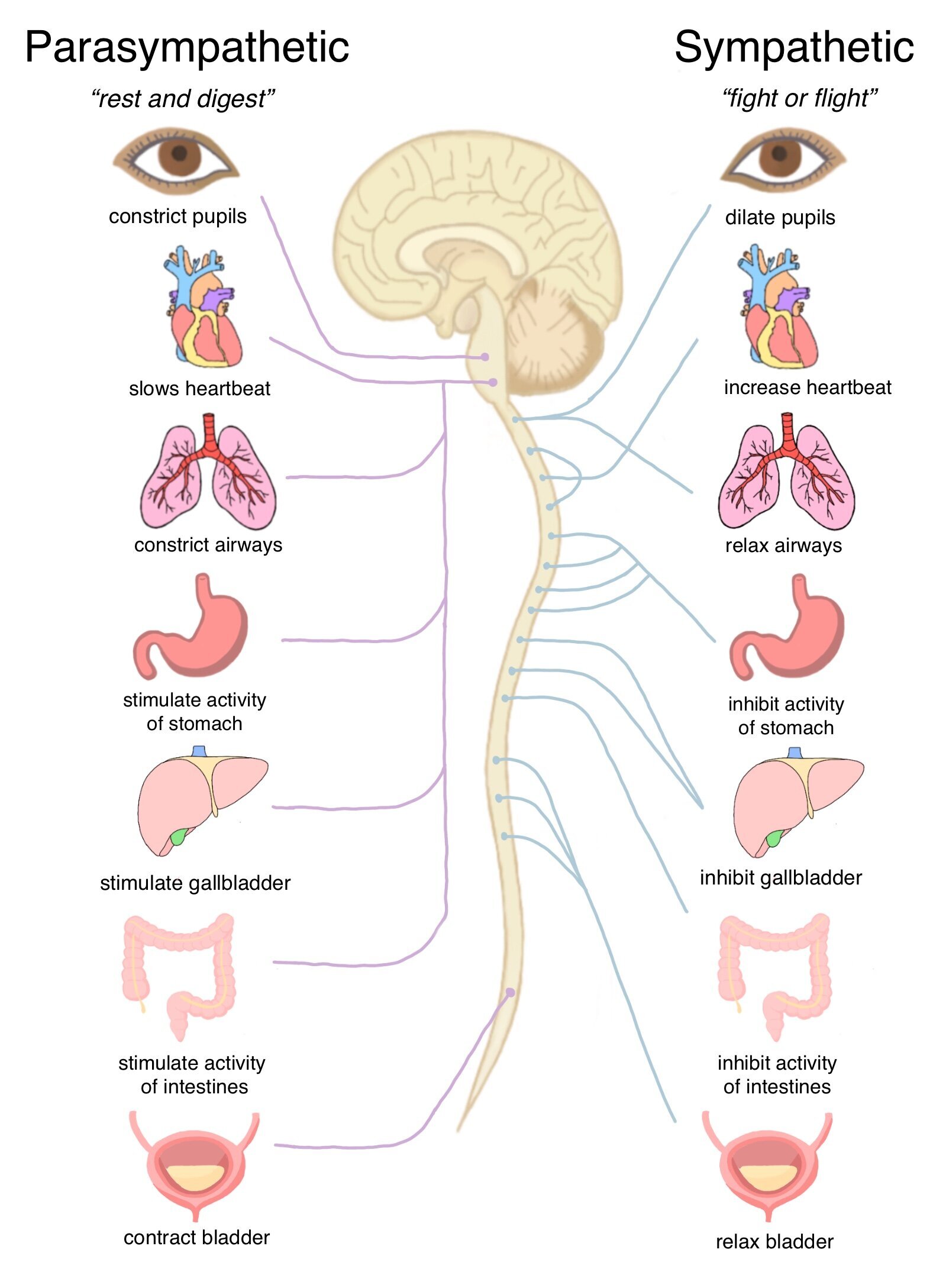
The ANS is the part of our nervous system that acts unconsciously and regulates involuntary bodily processes such as heart rate, blood pressure, breathing, and body temperature. The ANS comprises two parts: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS regulates our “flight or fight” response, while the PNS regulates our “rest and digest” response. The ANS requires a balance of these systems, and if one system, such as the SNS, is in overdrive, this results in ANS dysfunction.
Visual created by Lori Mae Yvette Calibuso Acob (2021 Concussion Alliance Intern), showing normal ANS is compared to ANS dysfunction.
While ANS dysfunction is a new research field regarding concussions, several studies have shown that “it is ‘likely’ that concussions cause autonomic nervous system anomalies.” Studies have also shown that one of the regions of the brain that may be negatively impacted by concussion is the midbrain.
The midbrain, located in our brainstem, is the central connection between the brain and the spinal cord. This region is where most ANS neurons are found. Since the midbrain is particularly vulnerable to the impact of concussions, it is concluded that damage to these neurons can affect the ANS.
To help better understand this problem, this page will explore the causes and symptoms of ANS dysfunction related to concussion, potential diagnostic tools, and options for treatment and therapy.
What is the Autonomic Nervous System (ANS)?
The autonomic nervous system (ANS) is a collection of neurons situated in our brain stem and spinal cord. The ANS functions unconsciously without voluntary control and comprises two systems: the sympathetic nervous system and the parasympathetic nervous system.
The sympathetic nervous system is our “fight or flight” response and is activated when we exercise, feel excited/embarrassed, or experience stressful situations. When we are in stressful situations, our sympathetic nervous system increases our heart rate and raises our blood pressure. It also functions in slowing bodily processes that are less important in emergencies, such as digestion and urination.
The parasympathetic nervous system, on the other hand, activates our “rest and digest” response. This system helps maintain our bodies and conserve energy for later. Our parasympathetic nervous system lowers our heart rate and blood pressure and increases digestion and urination.
Ideally, the ANS will balance the sympathetic nervous system and parasympathetic nervous system so that they are in equilibrium.
Visual created by Lori Mae Yvette Calibuso Acob (2021 Concussion Alliance Intern), illustrating the functions of the sympathetic and parasympathetic nervous system. Click on the image for a printable PDF.
Symptoms of ANS Dysfunction
ANS dysfunction, also called dysautonomia, develops when nerves in the ANS don’t communicate as they should. When the nerves in ANS don’t communicate properly, our bodily functions become less regulated. This ANS malfunction can lead to the overdrive of the sympathetic nervous system. Dysregulation can lead to heart and blood pressure problems, as well as exercise intolerance, persistent headaches, and insomnia.
Visual, created by Lori Mae Yvette Calibuso Acob (2021 Concussion Alliance Intern), displaying distinguishable symptoms of ANS dysfunction.
There are many symptoms of ANS dysfunction, and it can vary from person to person. A common symptom of ANS dysfunction or dysautonomia is orthostatic intolerance. This means you feel dizzy or faint when you stand up too quickly.
ANS dysfunction can also result in mental health difficulties such as anxiety and depression, increased stress levels, irritability, apathy, and nervousness. It’s important to note that if you have pre-existing depression or anxiety, a concussion could trigger another depressive episode or amplify existing mental health conditions. If you find yourself experiencing these symptoms, it is important to take steps towards caring for your mental and emotional wellbeing. It could help to keep a journal or mood tracker after getting a concussion to track how you are feeling throughout the day. Beyond Concussions also hosts monthly support groups and other forms of support can be found on our online support page.
Other symptoms include:
Exercise intolerance where you may have the inability to finish a workout because of worsening headaches or balance problems. This can also refer to your heart rate not increasing in an appropriate way the entire time you exercise, meaning that your heart is not doing its job of adjusting to activity level.
Sweating abnormalities such as hyperhidrosis in which you are sweating excessively. Abnormal or excessive sweating may occur in cool weather or entirely out of nowhere.
Irregular heart rate in which you may experience a resting heart rate that is either too low or too high. Other irregularities in heart rate may include difficulty getting the heart rate back down to rest or may experience heart palpitations.
Frequent headaches or migraines.
Insomnia where you have difficulty falling or staying asleep. You may also experience sleep disruptions where you are waking up panicked or sweating.
Difficulty digesting food or changes in metabolism/eating habits such as feeling dull after a few bites, loss of appetite, diarrhea, abnormal bloating, or difficulty swallowing due to heartburn.
Urinary problems such as difficulty using the bathroom, incontinence, inability to sense a full bladder, and inability to empty it completely.
Sexual difficulties such as men being unable to maintain an erection or being able to ejaculate, or women feeling dryness or low libido.
Good podcast – ANS in concussion
Potential diagnostic tools for ANS dysfunction
Since ANS and ANS dysfunction differs for each person, there is no standard diagnosis for ANS dysfunction. Many providers use a holistic approach to diagnose ANS dysfunction instead of focusing on a single variable. Thus, the ANS can be measured in a variety of ways. These measurements will provide insight into how well the ANS is functioning and potential indicators of ANS dysregulation.
Concussion-related ANS dysfunction diagnosis
Heart Rate Variability (HRV)
According to a systematic review by neuropsychologist Jon L. Pertab et al. and studies published in the Journal of Clinical Medicine and Neurology, a common measurement technique for concussion-related ANS dysfunction includes heart rate variability (HRV). HRV measures the average variation in time between each heartbeat and is typically used to assess if the heart is properly regulated. It is thought that:
The sympathetic nervous system increases heart rate and decreases HRV
The parasympathetic nervous system decreases heart rate and increases HRV
In practice, these systems of the ANS work in harmony to regulate heart rate and HRV for optimal heart functionality.
To measure HRV, your healthcare provider may use an electrocardiogram. This painless test will require you to have 3 electrodes placed on your chest, arms, and legs in order to measure your heart’s activity. Your HRV can also be measured at home using wearable technology. However, it is important to note that no agencies are currently regulating these at-home devices, and the devices may not be as accurate as they claim.
Buffalo Concussion Treadmill Test (BCTT)
Another test that is used to measure dysfunction after a concussion is the Buffalo Concussion Treadmill Test (BCTT). Commonly used with patients experiencing exercise intolerance, the BCTT is a stress test that is used to assess the subsystem threshold of aerobic exercise. For more information about the BCTT, see our page on Graduated Exercise Therapy.
Dr. Barry Willer of the University at Buffalo Concussion Management Clinic explains the procedure and nuances of the Buffalo Concussion Treadmill Test (BCTT).
Non-concussion-related ANS dysfunction diagnosis
According to the American Academy of Neurology (AAN), the following tests are standard techniques for ANS testing. However, these tests have not been clinically performed on individuals with ANS dysfunction caused by concussion.
Deep breathing test: This test is intended to measure how much your heart rate changes when you breathe in and out. When performing this test, you can expect to have electrodes attached to your chest to monitor heart rate and blood pressure cuffs on your fingers to measure your blood pressure. During the test, you will be asked to take slow deep breaths for one minute.
Thermoregulatory sweat test (TST): Sweat tests help evaluate your ability to sweat in a controlled, warm, and humid environment. During TST, a yellow dye is applied to your skin, and you will be placed in a closed, heated environment to stimulate sweating. As you sweat, the color of the dye changes to a bright purple, helping doctors evaluate your sweat loss patterns.
Tilt table test: Your doctor may recommend a tilt table test to trigger symptoms of lightheadedness, dizziness, or fainting. This test takes 45–90 minutes and helps assess any changes in blood pressure or heart rate.
Quantitative sudomotor axon reflex test (QSART): QSART is another sweat test used to measure the nerves that control sweating. In this test, your sweat glands will be stimulated as electrical currents are being passed through your legs and arms. If performing this test, there may be a slight burning discomfort experienced at the site of stimulation.
Valsalva maneuver: The Valsalva maneuver is a breathing technique that tests how well your heart is working by measuring your heart rate and blood pressure. This test is similar to popping your ears—pinching your nose, closing your mouth, and exhaling as if we were blowing a balloon. The only difference is that now we are bearing down as if we are using the bathroom. Your doctor may recommend this test to measure heart rate and blood pressure.
What treatment or therapy options do I have?
Although there is no cure for ANS dysfunction, treatment can help you manage your symptoms and improve your quality of life. Your treatment plan may include:
Vestibular Rehabilitation Therapy (VRT): In an interview with Sarah Gallagher, PT, DPT, NCS, she says that “...vestibular therapy is an excellent start because it has such a strong connection to the autonomic nervous system...”
In VRT, your therapy is individualized for your needs and may include:
balance/walking exercises
motion sensitivity exercises
sport or work-specific exercises
eye exercises
In the case of ANS dysfunction, your PT will look at your triggers of high sympathetic nervous system drive and teach you to recognize these symptoms. Then, they will introduce you to exercises to subdue your sympathetic nervous system and bring your ANS back to a balance.
See our page on Vestibular Therapy which has instructions on how to find a vestibular therapist.
Biofeedback Therapy: In biofeedback therapy, you will learn techniques to engage with your parasympathetic system, which will promote greater balance within the ANS and alleviate symptoms. One form of biofeedback therapy is heart rate variability biofeedback (HRV-B).
HRV-B focuses on metronomic breathing techniques to elicit a parasympathetic response by synchronizing your breathing with your heartbeat. This synchronization is called resonance. In resonance breathing, you will be trained to control physiological processes such as blood pressure and heart rate to restore ANS balance. This breathing technique will allow you to reduce activation of the sympathetic nervous system and increase control of the parasympathetic nervous system, bringing ANS to balance.
This video explains the concept of HRV and how resonance breathing can be beneficial for individuals with high sympathetic nervous systems.
Graduated Exercise Therapy: Research indicates that that graduated exercise therapy is a viable treatment option for those experiencing concussion-related ANS dysfunction. Physical deconditioning can prolong concussion-related ANS dysfunction recovery. Thus, after the initial resting stage (24-48 hours), it is important to regularly and gradually increase your physical activity without exacerbating symptoms.
See our page on Graduated Exercise Therapy.
Symptomatic Treatment and Life Changes: In some cases, your healthcare provider may target specific symptoms affecting your body the most. Although these treatment options are not proven to help with concussion-related ANS dysfunction, they are recommended to help alleviate symptoms brought by ANS dysfunction itself. Such treatments include changes to diet and new prescriptions for medication.
What happens to the brain at the cellular/molecular level when ANS dysfunction is present?
According to new research, the midbrain is a good indicator of how impactful the concussion was on the brain. This is also true for repetitive sub-concussive hits, such as those experienced by contact sports athletes. For three years, researchers studied a group of college football players before and after their athletic season. Researchers "scanned the players' brains in an MRI machine before and after a season of play," and the athletes wore helmets fitted with impact sensors. The study compared the correlation between decreased amounts of midbrain white matter and the severity of head impacts. The research team found that the number of hits sustained to the head correlated with the extent of white matter damage in the midbrain. Only two players were diagnosed with a concussion during the study, but "more than two-thirds of the players experienced a decrease in the structural integrity of their brain."
Moreover, the researchers discovered that the rotational acceleration—the head twisting side to side or front to back—had a stronger link to white matter degradation in the midbrain than linear acceleration, otherwise known as head-on impact. These findings highlight that the midbrain region is highly vulnerable to damage due to concussion and repetitive subconcussive hits. The midbrain controls several functions that can be thrown out of balance after a concussion, such as visual tracking, auditory perception, and our autonomic nervous system.
Exploring key features of the brain may also help suggest additional possibilities as to why it is difficult to diagnose ANS dysfunction after a concussion. Neurons are specialized cells that serve as the working units of the brain: they transmit information to other neurons, muscle cells, and glands. Neurons contain unique components that we can't find in other cells in the body: dendrites, axons, and synapses. Dendrites are branch-like structures that extend from the cell body (soma) of the neuron and are responsible for receiving messages from other neurons and sending that information to the cell body. The axon is a tube-like structure that acts as a "freeway" where electrical impulses, or messages, travel between neurons. Synapses are not actual structures on the neuron but rather gaps that serve as chemical junctions between axon terminals and dendrites of different neurons. To better visualize this structure, imagine a game of telephone using two cups and a string connecting these cups.
The cups represent our dendrites—it is where we speak the message into; thus, it's where the message is received. The string that connects the two cups is our axons—the message we speak into the one cup travels down the string to the other cup. The area where the string and cup connect is our synapse—this junction is where the axon and dendrites of different neurons interact.
Neurons collectively make up neural networks and the nervous system. Electrical impulses are transmitted in a pathway, simplifying the impulse moving through axons to dendrites via synapses. Think of the game "hot potato," where people are in a line or a circle beside each other: the hot potato is the electrical signal, and the people are the neurons.
Try to recall a time you have touched something hot. You probably jumped back in surprise or jerked your hand back in response. This is because the neuron in your hand received a signal that the object was hot and sent that message to your brain. However, that one neuron in your hand cannot send that signal to your brain on its own—it needs to communicate with its neighboring neurons to send that signal to your brain.
The game of hot potato resembles this communication system between neurons! The "hot potato" is the "hot" signal, and the people involved are the neurons. When one person receives the hot potato, it quickly sends this hot potato to another person. And that person sends the hot potato to another person and so on.
This system is, and has to be, instantaneous to promote effective and essential communication between the nervous system and the rest of our body. Thus, it is vital that the body must maintain communication so that bodily processes proceed accordingly. However, if one neuron cannot interpret the signal, it will not pass to its neighbor neuron. If this signal is not interpreted correctly, this can cause miscommunication between neurons and affect how well our body can function. When this happens, it can result in ANS dysfunction.
To look at this idea more closely, our ANS contains visceral efferent pathways that supply nerves to smooth muscles, cardiac muscles, and glands. For an example of these muscles and glands, common smooth muscles include the stomach, intestines, and bladder; cardiac muscles include our heart, and glands include our sweat glands.
The visceral efferent pathway involves clusters of autonomic nerve cells, called the autonomic ganglion, each with two neurons and a synapse. The autonomic ganglion is divided into smaller groups of ganglions that share nerves extending in similar locations and functions. For example, one group of ganglions within the autonomic ganglion is called the superior cervical ganglion which contains many nerves found in the head. The celiac ganglion is composed of nerves located in our abdomen and the inferior mesenteric ganglion has nerves that extend to our reproductive organs.
Visual, created by Lori Mae Yvette Calibuso Acob (2021 Concussion Alliance Intern), illustrating the different organs found in specific autonomic ganglion groups.
The two neurons involved in the autonomic ganglion are the preganglionic neuron and the postganglionic neuron. The preganglionic neuron is located in the brainstem or spinal cord, and the postganglionic neuron is located in target organs such as those mentioned previously. These neurons meet in a specific ganglion group within autonomic ganglia and must work in order to have a functioning ANS. Where they meet in the autonomic ganglia relates to their specific function and the division of the autonomic system they’re serving.
If one neuron, such as the one in our brainstem, cannot interpret signals correctly, the specific neuron on the organ it is synapsed with will not get that message. As a result, our bodily processes cannot function normally. For example, if a neuron in our brainstem synapses to a neuron in the heart but cannot interpret signals correctly, it can cause an irregular heart rate. Similarly, if the neuron synapses to your bladder, this can cause various problems, such as the inability to sense a full bladder or the inability to empty it completely. Ultimately, this will lead to ANS dysfunction.