Workers & Workplaces
Workplaces can be stressful and demanding environments; an employee may work long hours, experience fast-paced working environments, and carry out complex tasks requiring attention to detail. This page specifically addresses a concussion’s impact on work life and how to return safely to work.
Overview
A concussion, also called a mild traumatic brain injury (mTBI), is often overlooked as a trivial injury, as many regard recovery to be quick. However, many concussion patients do not recover in a quick or linear way, and some people develop persisting symptoms that require rehabilitation. Furthermore, concussions are “invisible,” meaning that diagnosing and treating may be complicated by symptoms and signs that aren't always easy to recognize. Therefore, concussions must be taken seriously. In this page, we will use the term “concussion” to refer to this type of brain injury.
Whether a concussion is sustained on or off the job, the demands of work can complicate things. Workers may need to take special precautions to ensure a safe return to work. Once back at work, workers may struggle to return to their work at full capacity or perform their usual tasks. Furthermore, socioeconomic factors play a role in a worker’s ability to recover before returning to work. A concussion can seriously impact a person's source of income, making it difficult to not only pay for necessary medical care, but also to afford basic necessities.
Some estimates show that about one in four concussions in adults occur while at work. A concussion received while at work will follow a slightly different process than one that occurs outside of work, usually requiring an injury-reporting protocol implemented by the employer. Regardless of where and how the concussion is sustained, the symptoms and recovery process will likely affect work life.
A worker who sustains a concussion must be willing to advocate for themself so that the concussion recovery process is as efficient and effective as possible and minimizes risk for persisting symptoms after concussion. Workers may need to advocate for work accommodations or make adjustments to their working style, role, or location (as possible). Information about workers’ compensation can also be found further down this page. The return to work timeline will vary for each individual, based on severity and symptoms of the concussion, as well as many other factors. Concussion Alliance’s Recovery Guide explains the general process of recovery, while a return to work timeline tailored to workers specifically can be found below.
Workplace Concussions
Concussions can impact someone’s work life whether or not the injury happens at the workplace. However, concussions on the job are very common: about 25% of adult concussions may happen at the workplace.
How do concussions happen in the workplace? In general, the most common causes of concussions are falls, hits to the head, or vehicle crashes in occupations involving driving. Concussions can happen in any workplace; however, some workplaces are more dangerous than others. For example, construction jobs have the most traumatic brain injuries among US occupations, with falls being the most common cause. In commercial warehouses and in agricultural settings, machinery accidents involving lifting machines like forklifts or agricultural machines like combines can also occur. Not all workplace concussions occur from accidents: military personnel, law enforcement, and emergency medical workers are all at risk of concussion from violence; in fact, 73% of workplace violence occurs against healthcare workers.
If a concussion occurs in a workplace, the immediate response should be to inform a supervisor and follow guidelines that are consistent with current best practices to determine if immediate medical attention is needed. If the worker has “red flag” symptoms, they should be taken to the emergency department. Regardless, the injured person should be removed from the worksite immediately to prevent a repeat blow. If they do not have red flag symptoms, they should see a medical provider (usually a general practitioner) within 48 hours of their concussion. Their general practitioner can make sure the worker does not have a more serious brain injury (such as bleeding in the brain) or injury to the neck, monitor the patient through their concussion recovery process, and give referrals for rehabilitative care. Workplaces should report the injury to their worker’s compensation carrier within 24 hours, and workers may want to follow up with their workplaces through text or email to make sure this gets done.
Figure from the online Concussion Awareness Training Tool (CATT). Can be used to guide your response to a concussion over the first 48 hours.
It’s vital for the workplace to be empathetic and communicative with the concussed employee. Workplaces should encourage workers to return to work safely and with appropriate accommodations, and managers should make sure they maintain a workplace environment where workers feel comfortable asking for accommodations or time off. There is no set timeline for concussion recovery, and while most people recover within a few weeks, others may experience persisting symptoms (defined as symptoms lasting more than four weeks) that can impact their life both inside and outside of the workplace.
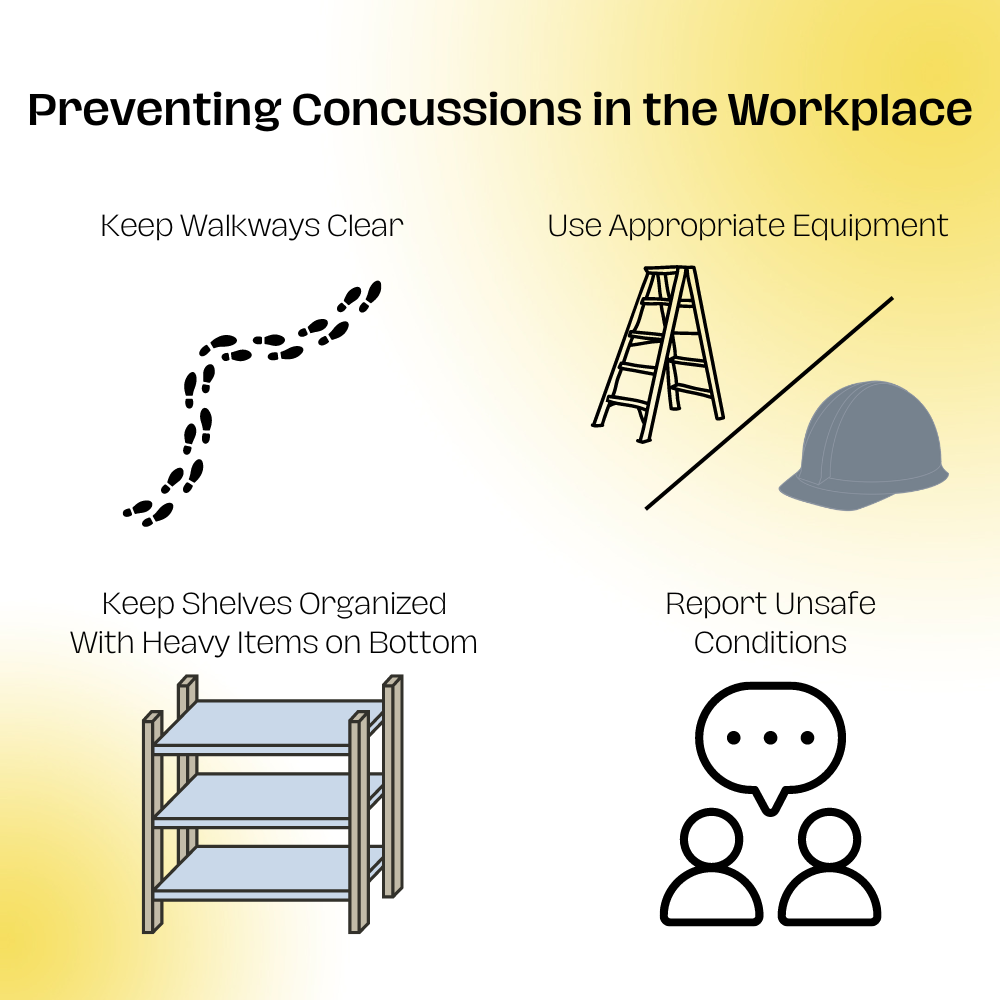
Prevention
Workplaces should also take proactive steps to prevent concussions. A series of online educational resources for concussions produced by the Concussion Awareness Training Tool (CATT) includes these important prevention measures in their Workers and Workplaces course:
Removing tripping hazards. Walkways and workspaces should be free of clutter, cords, puddles of water, or anything else that can cause a fall
Keeping shelves organized with the heaviest items on the bottom
Using proper signage to mark wet areas
Clearly marking low-hanging obstacles
Using ladders or step stools instead of chairs, tables, etc.
For workplaces involving driving, limiting driving hours to prevent fatigue
Providing adequate security, training, and emergency communication methods to prevent violence (when relevant)
Wearing hard hats correctly, meaning helmets are properly fitted and in good condition. New developments in hard hat technology are increasing the effectiveness of protective headgear. While newly designed hard hats may prevent more severe head trauma like skull fractures, no definitive studies show that hard hats prevent concussions.
Encouraging employees to report any unsafe conditions
Return to Work Basics
The Concussion Awareness Training Tool provides a step-by-step guideline for returning to work. Below we’ve provided the first stage, with a note on how these guidelines might be modified by the recently-published 6th consensus statement on concussion in sport. We explain the full guidelines in our Return to Work Explained section below.
CATT Return to Work Guidelines–Stage 1 (first 24-48 hours)
During the first 24-48 hours after a concussion, you should rest in a calm and quiet environment, maintain a regular sleep schedule, and avoid activities that worsen symptoms by more than 1-2 points on a 10-point scale (based on your impression of symptoms).
Do not engage in any activities* that cause you to break a sweat or which cause an increase in heart rate. You can engage in, but try to limit, social visits (for example, friends and family) and the amount of time you spend on your phone, computer screen, or reading.
Before operating a vehicle, make sure to speak to a licensed medical professional in order to ensure that you are safe to drive.
Move on to Stage 2 when symptoms are improving or after 48 hours of rest, whichever comes first.
*Note: There are new guidelines about what to do the first 24-48 hours after a concussion. While the new guidelines were written for athletes, they may apply to workers. The 6th Consensus Statement on Concussion in Sport recommends “relative rest,” not complete rest. “Relative rest” includes doing daily activities, limiting screen time, and engaging in light-intensity physical activity. Please read these important details about “relative rest,” and how to do light-intensity physical activity during the first 24-48 hours.
Advocating for Yourself and Requesting Accomodations
The effects of a concussion can be difficult to navigate, and it is important to take the necessary steps in order to ensure a safe return to work. Sustaining a concussion at work or sustaining one outside of work will have different trajectories. How one advocates for oneself will be different depending on whether you are in the workers compensation system or not. Specifically, sustaining a concussion at work will involve navigating workers compensation. Workers will immediately be involved in a workers compensation process with a case manager. Each state has a different process for workers compensation, and we will cover more information regarding workers compensation in a section below.
Obtain medical documentation from your healthcare provider
When communicating with your employer, make sure to provide any medical documentation you may have received from your healthcare provider. Medical documentation should include information about the diagnosis and recommendations for managing the recovery process, including restrictions or accommodations. Your healthcare provider may fill out a medical assessment letter for you to take to your employer, or it may be beneficial for you to bring a template letter to your appointment. This template is a good example of what may be useful to bring to your healthcare provider to fill out: CATT Medical Assessment Letter. Once your healthcare provider fills this out, you can bring it to your employer.
Communicating with your employer and your co-workers
When requesting accommodations from an employer, be transparent about your situation and remember that your employer may not understand the severity of your injury. Be patient and explain everything clearly. Coming prepared with resources and documentation from your healthcare provider for your employer to understand how best to help you.
How to talk to people:
Be Transparent: Tell your employer or co-workers how they can best support you. This doesn’t necessarily mean you should divulge all details; telling others about your symptoms is your choice and dependent on context. Additionally, telling your employer about your concussion is private information; managers or supervisors are legally bound to keep medical information confidential and not share the details with anyone else.
Explain Accommodations: Your employer may not understand why you need a particular accommodation, and your co-workers might be confused why you get “special treatment.” While you are legally not required to disclose any of your symptoms, you may find it helpful to do so in the right environment. Explaining the symptom that you are experiencing in relation to an accommodation may help others to understand why it is necessary. However, if you don’t feel comfortable doing so, you can always tell fellow co-workers that your healthcare provider recommended these accommodations.
Provide a Note from Your Doctor: Having documentation from a medical professional will allow others to see the gravity of your situation. A healthcare provider can also provide recommendations for accommodations which can be helpful in convincing your employer of the necessity of those accommodations.
Communicate Frequently: Your symptoms may fluctuate fairly often, as progress is not linear. Keep those around you informed as needed.
Be Patient!: Not everyone will understand right away and that’s okay. Just be sure to be patient and remind people gently what you are going through. Feel free to send them resources such as this one so that they can understand better.
Make a Plan: Your employer will want to know how they can help you. While you may not be able to provide them an exact timeline, the best way for your employer to support you is to follow your healthcare provider’s recommendations. Explain to your employer exactly what accommodations you need to do your best work as instructed by your provider.
Accommodations to request
Helpful accommodations are based on individual factors–both the worker’s symptoms and the environment/job role factor into finding appropriate solutions for returning to work safely. Below is a list of possible accommodations that your healthcare provider might recommend or that you can request in order to alleviate some of the symptoms:
Change of office space or location to reduce distraction
Restructure job schedule or hours
Telework
Additional time to complete tasks
Reduced hours
Flexible schedule
Working with your supervisor to implement these effectively is important. The Job Accommodation Network is also a helpful tool to think about what accommodations might work for you and is also something you can recommend to your healthcare provider or employer. It provides a wide variety of possible accommodation arrangements categorized by the employee’s limitations and by work-related function.
The methods you use to address your symptoms might also vary based on your job. For instance, physically demanding jobs, jobs without breaks (teachers), or jobs with fluorescent lighting (hospitals) might require more or different symptom management strategies and may be more difficult to return to. Construction workers and similar professions might need to start out working just a few hours or days a week, especially if the environment triggers light and noise sensitivity. In some cases, workers with physically demanding jobs (construction workers) can sometimes benefit from moving to office or paperwork roles while recovering from an injury. Of course, these alternate roles may require further accommodation needs as well. In any case, all jobs pose unique challenges, and workers should engage with managers or human resources to determine the best course of action.
Self-Managing Symptoms at Work
While accommodations are things you need to ask your workplace or manager for, there are also ways to self-manage your symptoms on the job. Workplace-provided accommodations can go a long way, but finding methods to manage some of your symptoms on your own can be incredibly helpful. Below is a list of symptoms and possible ways to address them. Try a variety of methods until you find some that work for you; everyone’s needs are different. You can also check out Concussion Alliance’s page on self-care.
Headaches, nausea, and dizziness:
If bothered by bright lights, try using sunglasses or a baseball cap. However, avoid wearing sunglasses indoors as it may exacerbate light sensitivity.
If noise causes headaches, try earplugs or noise-canceling headphones.
Be sure to get adequate nutrition, water, and sleep.
Look into medication for headaches.
Avoid motion such as elevators and vehicles if experiencing dizziness or nausea.
Some glasses (such as bifocals and varifocals) can cause problems; check out Concussion Alliance’s page on vision therapy for more information on vision issues.
Purchase a standing desk attachment if sitting for prolonged periods worsens headaches or neck pain. If standing can make you dizzy or lightheaded, be careful and keep a chair nearby so you can sit down if needed.
To reduce symptoms related to looking at computer screens:
Print materials instead of viewing them on a monitor.
Use a blue light filter for your screen.
Copy and paste text into a text-to-speech software such as Google Translate or Natural Reader so you can listen instead of read.
Take frequent breaks such as walking or pacing for a few minutes, practicing meditation or deep breathing with your eyes closed, doing prescribed physical therapy exercises, etc..
Mental strain:
Prioritize tasks, doing the most important things first.
Make a to-do list or schedule (if you’re having trouble with organization, you can reference Concussion Alliance’s page on cognitive dysfunction).
Manage the expectations of others (managers, co-workers, friends/family)—they may not understand the impact that concussions can have.
Break up tasks with breaks, and recognize that many things may take longer than you’re used to.
Maintain a calm environment, such as working in a room without other people or without too much clutter. Complex visual fields can be very challenging, so decluttering can often help reduce fatigue and overstimulation.
Set scheduled reminders to eat using an online calendar or something similar; loss of taste and smell can lead to a reduced appetite and a lack of interest in food.
It also may be helpful for a worker with a concussion to have a conversation with their co-workers. Employees with concussions who perceived co-workers as supportive generally thought this contributed to a less stressful return to work process. A sympathetic and understanding social support system can improve working conditions and the recovery process. Social support from friends, co-workers, and managers is also critical; you aren’t alone in your recovery, and the people around you want to help. If you want to convey the wide-ranging effects of concussions to your peers, you can check out some personal stories here.
Workers' Compensation, Insurance Coverage, and Time Off
Worker’s Compensation
Workers’ compensation is the provision of wage replacement, medical treatment, vocational rehabilitation, and other possible benefits to employees who have suffered injury or illness. Federal employees or their dependents may look for more information on the Federal Employees’ Compensation Program and are eligible to file a federal claim. For others, workers’ compensation programs vary state-by-state, but anyone who suffers an injury due to their work (and who is employed by a company with workers’ compensation insurance) is eligible to file a workers’ compensation claim. Check this link for a 2023 review of state-by-state workers’ compensation laws, and use this link to find more detailed information on state-by-state policies.
Workers’ Compensation Often Covers the Following:
Medical Benefits
workers’ compensation should cover all costs associated with diagnosing and treating a work-related concussion
Temporary Disability
if you are unable to work at all or can only work in a limited capacity due to your concussion and resulting symptoms, you may file for disability benefits for the time it takes you to return to work
When filing for workers’ compensation, it is important to be aware of the primary arguments used to deny claims for concussions. Claims are often denied because the employee did not notify their employer of the incident within thirty days of it occurring, or did not file their workers’ compensation claim within two years. Additionally, failure to seek medical treatment promptly following the injury or a lack of medical records addressing the injury are common reasons a workers’ compensation claim is denied. Filing the proper paperwork and having physicians’ notes documenting your symptoms can help support your workers’ compensation claim.
It does not matter if you or your employer are at fault for the injury when filing for workers’ compensation. If an employee receives workers’ compensation benefits, they lose the right to sue their employer for the injury.
Oftentimes hiring an injury lawyer can help in the process of filing for and receiving workers’ compensation. They will understand your states’ policies and can follow up with your employer or the government to ensure your claim is being processed in a timely manner.
Medical Insurance
As mentioned above, workers’ compensation is only available to those injured at work and whose employer has workers’ compensation insurance. However, those who do not qualify for workers’ compensation will receive coverage for concussion care if they are enrolled in a health insurance program. If your primary care provider determines you will need further assistance in your recovery, you may ask them or your insurance company the details of what care is covered.
Physical symptoms (including those from concussion) are generally covered by insurance and considered medical problems. Mental health concerns that result from a concussion may be covered in your insurance’s mental health benefits package, although this is oftentimes more limited than physical symptom coverage.
Medicare
Medicare is a federal health insurance program for those over the age of 65 or living with certain disabilities. If you are required to file a claim for Medicare coverage, it is vital to submit your claim with all the documentation possible, including medical bills, physicians’ notes, and more.
Medicare Part A covers inpatient services and hospital stays. Medicare Part B covers outpatient services and equipment. Medicare will cover, partially or fully, the costs directly associated with treating your concussion. Learn more here about using Medicare with workers’ comp.
Medicaid & the ACA
Medicaid is a federal program that provides health insurance to low-income citizens, and is administered on a state-by-state level. The Affordable Care Act expanded eligibility requirements for Medicaid coverage. You can read about your state-specific policies here.
Affordable Care Act (ACA)
The Affordable Care Act (ACA), otherwise known as PPACA, is a law that expanded healthcare coverage for many people. You can enroll in health care through your state and see if you are or can be covered here.
Family and Medical Leave Act (FMLA)
The Family and Medical Leave Act (FMLA) allows for an employee to take up to 12 weeks of leave for medical reasons, with some restrictions. Leave may be unpaid or used concurrently with employer-provided paid leave. Under the FMLA, employers are obligated to continue all group health benefits for the employee. Employees are guaranteed their same position upon return, or a near-identical position. Medical leave due to inability to work, inability to perform an essential function of your job, and work leave to attend healthcare visits as a result of symptoms following a concussion is protected under the FMLA. More information regarding the definition of a serious medical condition by the FMLA can be found here, and information regarding eligible employees can be found here. The FMLA is a federal law; however, some states have their own FMLA laws; you may need to look up whether the laws differ in your state.
What if Symptoms Persist?
A 2022 study found that half of people with a concussion “reported three or more symptoms at a year after their injury, and >70% reported at least one problematic symptom.” Additionally, a 2019 Canadian study found that 80% of workers who’d visited the emergency department for a concussion missed at least one day of work, and while almost all (91%) of them returned to work within 90 days, almost half (41%) reported persisting symptoms. Workplace fatigue and an inability to maintain one’s previous workload are common problems. However, societal understanding of concussions as serious and possibly long-term injuries is limited. Even if workplaces are accommodating for the first few weeks, they might become less understanding if concussion symptoms persist.
It is even more important to advocate for yourself if your symptoms persist; persisting symptoms are defined as symptoms lasting more than four weeks. If you’re struggling to recover, refer to the accommodations and managing symptoms sections for suggestions, or our section on getting more help below. You might need to speak with a manager in your workplace a second time to ensure longer-term support from your workplace.
ADA & Social Security Disability
Americans with Disability Act (ADA)
The Americans with Disability Act (ADA) protects employees from being discriminated against on the basis of disability. ADA requires that an injury must be of substantial duration with long-term effects in order to qualify as a disability protected by the ADA rights. Critically, the ADA applies to long-term symptoms: employers may be required to provide reasonable accommodations to help employees with concussions whose symptoms persist. According to the U.S. Equal Employment Opportunity Commission, a substantial and long-term impairment is defined as impairment in performing a major life activity such as “hearing, seeing, speaking, breathing, performing manual tasks, walking, caring for oneself, learning or working.” In this case, “the individual may suggest a reasonable accommodation based upon her own life or work experience. However, when the appropriate accommodation is not readily apparent… [the employer] must make a reasonable effort to identify one.” This definition means that these rights may apply to workers who experience persisting symptoms after concussion (PCAS) that significantly limit their ability to perform their normal daily tasks.
If you qualify for the ADA, employers are legally required to provide you with reasonable accommodations, with some exceptions. Concussion Alliance does not give legal advice, and we recommend that you consult an attorney.
Social Security Disability
To qualify for Social Security Disability (SSD), one typically must expect to be out of work for at least one year due to their disability. However, some state programs (unrelated to SSD) support people with partial or short-term disabilities. The Social Security Disability Benefits document details the typical requirements to qualify for this insurance coverage and the usual benefits received.
Additionally, it typically takes 3-6 months, and often more time, to process SS Disability applications. Applying for Disability is a long, complicated, often tedious and challenging process. However, if persisting symptoms after a concussion are impacting your ability to work for a significant period of time, it may be worth pursuing.
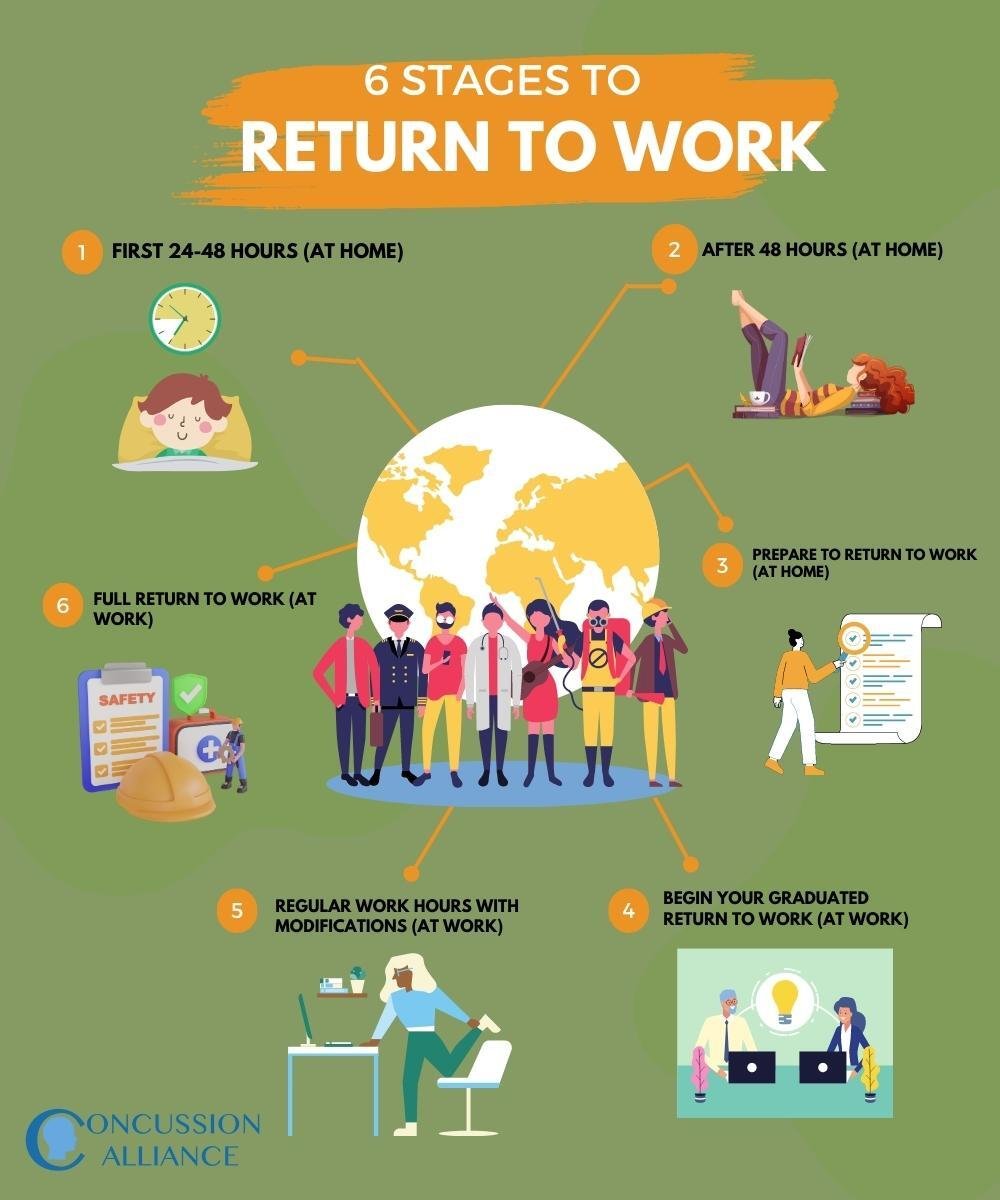
Return to Work Explained
For most, returning back to work, especially after an injury, can sometimes be difficult; returning to work might make some feel overwhelmed or afraid. When you are ready to get back to work, the following guideline should be helpful in supporting a smooth return to work. The following return-to-work guideline is adopted from the Concussion Awareness Training Tool (CATT).
This guideline has six stages for returning to work; you must successfully complete each one before moving to the next. CATT specifies that “after Stage 2, if new or worsening symptoms appear at any stage, go back to the previous stage for at least 24 hours. You may need to move back a stage more than once during the recovery process.” It is important to note that recovery is non-linear, and it is normal to return to a previous stage.
Stage 1 (At Home): The first 24-48 hours
During the first 24-48 hours after a concussion, you should rest in a calm and quiet environment, maintain a regular sleep schedule, and avoid activities that worsen symptoms by more than 1-2 points on a 10-point scale (based on your impression of symptoms).
Do not engage in any activities* that cause you to break a sweat or cause an increase in heart rate. You can engage in, but try to limit, social visits (for example, friends and family) and the amount of time you spend on your phone, computer screen, or reading.
Before operating a vehicle, make sure to speak to a licensed medical professional in order to ensure that you are safe to drive.
Move on to Stage 2 when symptoms are improving or after 48 hours of rest, whichever comes first.
*Note: There are new guidelines about what to do the first 24-48 hours after a concussion. While the new guidelines were written for athletes, they may apply to workers. The 6th Consensus Statement on Concussion in Sport recommends “relative rest,” not complete rest. “Relative rest” includes doing daily activities, limiting screen time, and engaging in light-intensity physical activity. Please read these important details about “relative rest,” and how to do light-intensity physical activity during the first 24-48 hours.
Stage 2 (At Home): After 48 Hours
After finishing stage one, you should slowly increase your cognitive activities, for example, reading, tv watching, or using a computer. Continue incorporating light physical activities* into your day, for example, going for a walk, swimming, or even light house chores. Be sure to avoid activities that pose a risk for another concussion, especially where there is a risk of fall, collision, or contact (such as contact sports). Also stop activities before becoming out of breath.
As you slowly increase the activities, be sure to also make time to rest as needed while keeping napping to a minimum to reduce your risk for sleep issues.
Start thinking about and planning your return to work. For example, think about how you will contact and communicate with your employer, your potential return to work plan, and whether you will need to make adjustments to your commute to work.
Before moving on to stage 3, make sure at least “30 minutes of activity is *tolerated”.
*Note: The 6th Consensus recommends that individuals begin light physical activities immediately after a concussion. After 48 hours, the 6th Consensus recommends that individuals begin to increase the intensity and duration of this activity. In the 6th Consensus, tolerated means that the activity does not worsen symptoms by more than 1-2 points on a 10-point scale for more than one hour after stopping the activity.
Stage 3 (At Home): Prepare to Return to Work
Stage 3 is preparing to return to work. Gradually increase your cognitive activity, such as reading and using the computer. Continue to gradually get back to activities from your daily routine, such as gardening or grocery shopping.
Try commuting to work (such as driving, walking, or public transportation) in order to assess if your usual commute aggravates symptoms or drains your energy in a way that would make it difficult to perform work tasks. You may need to consider commuting in a different manner, such as taking public transportation if the complex visual field of driving feels unsafe or fatiguing. You may also need to consider requesting to work from home or work at a different location, work shorter days or fewer days per week, or request a delay in your return to work.
A regular sleep schedule can support you with a successful transition to return to work.
Before returning to work, make sure you have had a discussion with your employer about accommodations which can include: flexible hours, reduced hours, reduced days per week, reduced workload, extra time to complete tasks, or a quiet and distraction-free environment to work.
Additionally, as you return to work, make sure to listen to your body and pace yourself. You should communicate with your employer about a plan to leave work and return back to Stage 2 if your symptoms worsen.
You can move on to Stage 4 once a total of 4 hours of non-work activity is well-tolerated (less than 1-2 point symptom increase out of 10) with breaks as needed.
Stage 4 (At Work): Begin Your Graduated Return to Work
Begin your return to work plan that you have agreed upon with your employer. This may mean returning to work with accommodations, including your agreed-upon number of hours a day of work, reduced workload, additional time to complete tasks, or access to a quiet or distraction-free workspace.
As you return to work, listen to what your body says and pace yourself accordingly. Prioritize less demanding tasks and responsibilities and focus on getting back into a reduced version of your routine that doesn't overwhelm you.
As you continue to progress through your recovery, you can gradually increase your hours each week as your symptoms allow (or as deemed appropriate by your healthcare provider).
Once you feel comfortable and confident with regular working hours and necessary accommodations, you can proceed to Stage 5.
Stage 5 (At Work): Regular Work Hours with Modifications
As your symptoms decrease or resolve, continue to adjust your accommodations. To help you better understand whether accommodations are needed or not, phase them out one at a time in “trial” periods. These “trial periods” will allow you to test how well you can manage your tasks and responsibilities without each accommodation, as well as assess the impact they have on your work performance and well-being.
As you begin working with reduced accommodations during this stage, it is important to monitor your energy levels, not only during work but at home as well. When completing household tasks, or engaging in social or recreational activities, make sure to see how your body or overall well-being is affected by the decreased accommodations. If reduced accommodations at work make it harder for you to do other necessary activities of daily living or take care of yourself and your family, you may need to return to the previous level of accommodations.
As your work efficiency or productivity increases, make sure that you continue to communicate regularly and effectively with your employer or supervisor. This will ensure that you prioritize self-care and well-being, so you are able to fully return back to work.
Once you have been able to tolerate regular work hours with minimal accommodations, you can proceed to Stage 6.
Stage 6 (At Work): Full Return to Work
This is the final stage where you fully return to work. At this stage, you should have comfortably returned to your regular routine, including your normal level of work productivity, without any accommodations.
When returning to work, take into consideration your job’s environment and safety protocols. If your job has safety implications, such as your duties requiring operating heavy equipment, working at heights, or driving, you are advised to go to your healthcare provider to get medical clearance before returning to work.
Once you have completed Stage 6, you can complete your regular work duties without any remaining symptoms. If your regular work duties worsen symptoms (less than 1-2 point symptom increase out of 10), go back to stage 5.
Getting More Help
Learning more through Concussion Alliance resources
For some, provider-prescribed workplace accommodations may not be enough to allow individuals to return to work—especially for those whose symptoms persist or who have trouble performing activities of daily living outside of work. Concussion Alliance’s Recovery Guide provides an outline for proper care pathways to help with recovery and the best practices for getting help and building the best possible recovery plan.
To learn more about concussions and the ways they can affect you, visit Concussion Alliance’s About Concussions overview page. Also consider visiting Concussion Alliance’s Affected Populations page, which has population-specific resources for how concussions impact women and girls, individuals with pre-existing disabilities, veterans, college students, and survivors of intimate partner violence.
For those trying to find treatments for particular symptoms, Concussion Alliance’s Treatments overview page includes resources on medical and rehabilitative (as well as complementary and alternative) treatments. To find a healthcare provider for a particular treatment near you, Concussion Alliance’s Find Providers page brings together provider search tools from trustworthy organizations and includes helpful guides for using them.
For patients navigating higher symptom burden, slower recovery, or symptoms persisting more than 4 weeks, a concussion or outpatient rehabilitation clinic is most likely to provide multidisciplinary care consistent with current best practices. A 2019 Canadian study found that 80% of workers who’d visited the emergency department for a concussion missed at least one day of work, and while almost all (91%) of them returned to work within 90 days, almost half (41%) reported persisting symptoms. Concussion Alliance’s Concussion and Rehabilitation Clinics page has resources on how to find the right clinic.
Self-care is a vital part of any concussion recovery, and is particularly important for those waiting on referrals or appointments, or for individuals with limited or no access to healthcare services. Concussion Alliance’s Overview of Self-Care resource includes a variety of self-sufficient options to aid your recovery while helping you to learn how different kinds of self-care best benefit your healing process and your body. The page includes resources in five categories to assist you on your journey to recovery.
Sleep: Sleep is an essential part of recovery, and can be disturbed after concussion. This section provides advice on different ways to help you sleep better and a brief education on sleep problems after concussion.
Exercise: This section provides recommendations for physical activity after concussion, including recommended exercise, types of exercise to avoid, and population-specific recommendations.
Nutrition: This section provides different suggestions of foods to avoid and foods that will reduce inflammation in your body and help with recovery. This aspect of your health is important because the types of food you put into your body affect your health.
Sensory Sensitivity: This section focuses on two types of sensitivity (visual and auditory) and provides tips and tricks to help manage your sensory sensitivity.
Emotional Wellness: This section provides healthy life habits and tips to help you be at a better place emotionally in your recovery. If you find yourself struggling, you can check out Concussion Alliance’s resources on Mental Health and Mental Health Among High School Students after concussion. You can further learn about how concussion can impact your mental health, how to take care of yourself, and how to find providers if you want to get help.
Outside Support
Social support is also a crucial part of concussion recovery, especially for those who are struggling to balance returning to work with other necessary activities of daily living. If you are having trouble, don’t be afraid to reach out to trusted friends, family, partners, and co-workers. You can ask for help with daily tasks like grocery shopping, meal preparation, cleaning up around your living space, or driving. Beyond positively impacting recovery through helping you manage your energy, this assistance can provide rejuvenating companionship during a difficult time.
Your personal support network isn’t the only place to get the kind of support mentioned above. According to the University of Buffalo School of Social Work, social workers “are devoted to helping vulnerable people and communities work through challenges they face in everyday life.” Social workers provide support for medical patients and many other at-risk populations and could be a beneficial part of your support team.
These professionals can help you build a better self-care plan and support you as you navigate returning to work and other activities of daily living. Some concussion and outpatient rehabilitation clinics include social workers on their teams. Social workers are also employed in a variety of settings, including hospitals, schools, Veterans Affairs agencies, and counseling clinics. If you’re interested in learning more, we recommend this video from the Canadian Concussion Centre LiUNA Webinar Series about the role of social workers in concussion management.










The New York State Workers’ Compensation Board has created new guidelines for Traumatic Brain Injury (TBI). While some areas could be updated to reflect a more current and nuanced understanding of brain injury, the guidelines include all best-practice treatment modalities and emphasize the case-by-case, highly patient-specific nature of the injury.